Equitable AI use to reduce the impact of AMR and bacterial infections
Applying design thinking approaches in empowering Patent and Proprietary Medicine Vendors (PPMVs) with a conversational Artificial Intelligence (AI) tool to increase their understanding on the rational provision of antibiotics at the community level.
Mr Dumale Aadum Don, Chief Operating Officer, Corona Management Systems.
- Innovation
Antimicrobial resistance (AMR) poses a great threat to human health globally thereby affecting humans, animal, and the environment[1]. Bacterial AMR is a problem in all the regions of the world with the highest rates of prevalence in countries in sub-Saharan Africa[2]. About 73.4% of deaths were attributable to AMR in sub-Saharan Africa, a region with one of the highest burdens of infectious disease globally[3]. In Sub-Saharan African (SSA) countries, non-prescribed dispensing of antibiotics by Patent and Proprietary Medicine Vendors (PPMVs) has been flagged as one of the contributing factors to the widespread misuse of antibiotics[4]. PPMVs are an important source of care for the urban poor and in rural areas.
Gaps in knowledge among PPMVs have been extensively documented, including gaps in knowledge on testing and treatment protocols for infectious diseases needing antibiotics[5]. This creates a concern for the quality of services provided by PPMVs in these countries[6]. In many countries in Sub-Saharan Africa including Nigeria, Lesotho, DRC, and Kenya, PPMVs often dispense antibiotics whenever demanded with very little history taking and counselling. Most times these drugs are given to clients /community members without proper consultations thereby increasing antibiotic misuse and ultimately antimicrobial resistance.
Our primary beneficiaries refer to PPMVs, who are frontline health service providers in low- and middle-income country (LMIC) contexts. These PPMVs play a crucial role in providing healthcare services to communities, particularly in areas where access to formal healthcare facilities may be limited. Many PPMVs may lack access to up-to-date guidelines on the rational use of antimicrobials. Our solution provides them with a conversational AI tool that translates key health system guidelines into a user-friendly format. This will help PPMVs better understand and apply these guidelines in their practice, promoting the rational use of antibiotics and improving patient care. Our solution offers PPMVs a conversational agent that guides them through decision-making processes by providing tailored recommendations based on client information inputted into the tool. The user-friendly and accessible tool helps to enhance their capacity and improve the overall health outcomes of community members in the four countries.
Our secondary beneficiaries are the people who patronise these PPMVs, whom we refer to as clients. This solution will help improve the quality of care for clients who patronise these PPMVs. Ultimately, reducing antibiotic misuse in the four countries and improving the overall well-being of the community members who patronise these PPMVs.
- Proof of Concept: A venture or organisation building and testing its prototype, research, product, service, or business/policy model, and has built preliminary evidence or data
- Artificial Intelligence / Machine Learning
Our solution offers a variety of benefits to users, particularly patent and proprietary medicine vendors (PPMVs), who serve the urban poor and those in rural areas across the four implementation countries in sub-Saharan Africa. By making our solution accessible to PPMVs, we aim to address the inadequacy of formal training among these frontline healthcare providers, who are primarily responsible for the health of more than half of the population due to the frequent visits they receive. Our solution focuses on building the capacity of PPMVs to effectively utilise antibiotics within the communities where they are deployed. Through training and support, we empower PPMVs to make informed decisions regarding antibiotic use, thereby contributing to improved healthcare outcomes.
Our solution focuses on ensuring the effective utilisation of antibiotics within the communities where they are deployed. Our solution will reduce the prevalence of wrong administration and dispensing of antibiotics, thereby reducing AMR. Also, the data generated by our conversational AI tool will be utilised for research purposes, contributing to the body of knowledge on antimicrobial resistance and healthcare practices in low-resource settings.
Additionally, our solution will generate community-level data that will be used in policymaking and regulating antibiotic use.
Our approach to creating tangible impact revolves around meaningful engagement with various stakeholder groups and identifying pathways to scale our solution effectively. By applying human-centered design (HCD) approaches, we would ensure active involvement and collaboration with the Ministries of Health, Environment, and Agriculture throughout the implementation process and beyond. This collaborative engagement ensures that our solution aligns with the priorities, targets, and national guidelines, which will ultimately enhance its sustainability and scalability.
Furthermore, our solution focuses on deriving value for our community of patent and proprietary medicine vendors (PPMVs), by providing them with a pathway to engage with the solution consistently and sustainably. Through tailored training and support, we will empower PPMVs to utilise the solution effectively by giving accurate healthcare support based on the antibiotic guidelines, thereby improving their capacity to deliver quality healthcare services to their communities.
Moreover, the data sets generated through reporting from PPMVs will serve as a valuable platform for enhancing understanding of antibiotic usage in Nigeria, Kenya, Lesotho, and the DRC. This data-driven approach enables us to gain insights into antibiotic usage patterns, identify areas for improvement, and inform evidence-based policy decisions. Additionally, it will help in generating community-level data in the selected countries.
Over the next three years, we have a strategic plan to scale our solution and expand our impact in improving healthcare delivery in low-resource settings. We are going to scale up our solution using a horizontal approach, and as a result of this we will be introducing the solution to different sites in the four implementation countries in a phased manner. This will allow for a stepwise expansion allowing for the adoption of new these practices and further refinement of our solution across the four countries.
We intend to reach 100 PPMVs each in the four countries spread across 3 cohorts. Using the phased incremental approach, we intend to reach 20 PPMVs each (i.e. the first cohort) in the four countries in the first 6 months of the project implementation and 30, and 50 PPMVs respectively in the 2nd and 3rd phase of implementation.
Collaborating with these key stakeholders will foster partnerships to ensure the sustainability and scalability of our solution. It will enable us to tap into their expertise and resources to enhance the effectiveness of our solution and optimise its integration into existing healthcare systems. We will continue to work collaboratively to expand the deployment of our solution.
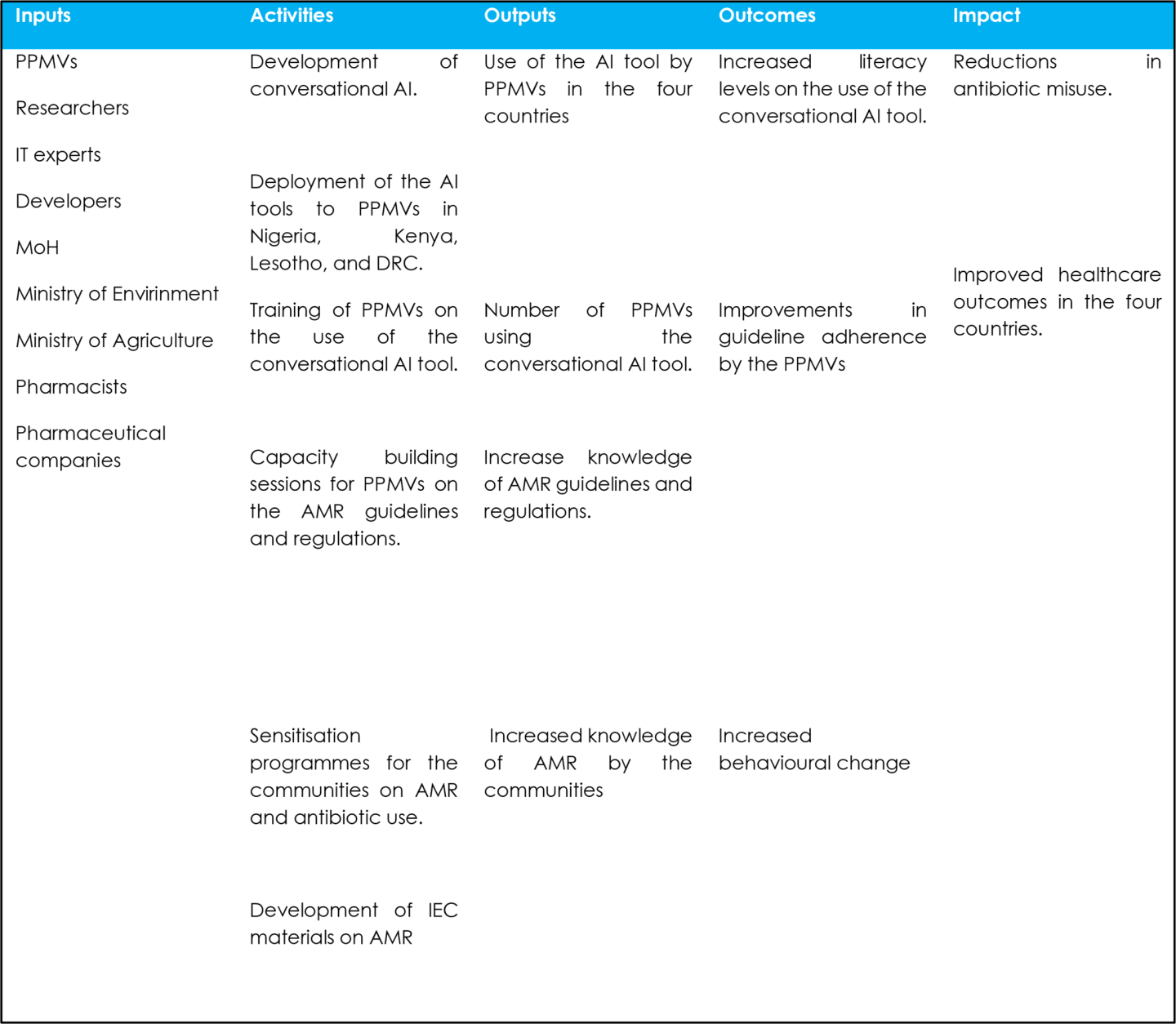
To measure success against our impact, we will be using our programme indicators, we will be using different methods to collect and track progress. This will enable us to track our progress towards achieving our project goals, which are to reach 100 PPMVs across 4 countries in 3 years, consisting of 3 different cohorts recruited using a phased approach.
Our output indicators include:
- Number of PPMVs in each country trained on and actively using the conversational AI tool. This will be measured using training records and the number of user logins across the four countries in 3 years.
- Number of PPMVs who have increased knowledge and understanding of AMR guidelines and regulations. This will be measured using pre- and post-intervention assessments/surveys collected periodically throughout the project implementation phase.
- Number of community members who have increased knowledge and awareness of AMR. These numbers will be obtained from the community data collected using FGDs/surveys across the 4 countries in 3 years.
Our outcome indicators include:
- Number of PPMVs' with increased literacy levels related to the use of the conversational AI tool.
- Number of PPMVs' adhering to the antimicrobial resistance (AMR) guidelines.
- Number of PPMVs' adopting the recommended practices following the intervention.
- Cameroon
- Canada
- Congo, Dem. Rep.
- Ethiopia
- Kenya
- Lesotho
- Nigeria
- Congo, Dem. Rep.
- Kenya
- Lesotho
- Nigeria
Resistance or scepticism from key stakeholders, including Ministries of Health, Local Governments, and community-based organisations, could impede the adoption and implementation of our solution. Lack of buy-in or support from these stakeholders may hinder our ability to effectively engage frontline health workers and achieve our goals. To address this, we will leverage our existing relationship with stakeholders building on our current work on LLM to simplify scientific communication in Sub-Saharan Africa including in Nigeria and Kenya.
Ethical and Bias Barriers: Conversational AI may present ethical challenges and biases due to the nature of their training data. To overcome this barrier, we will implement stringent bias detection and mitigation techniques throughout the training process. Additionally, we will diversify the training data to minimise biases. In addition to this, we may also experience a delay in obtaining ethical considerations. To mitigate this, we will leverage our existing relationships.
Security Barriers: Conversational AI is susceptible to security risks, such as adversarial attacks and potential misuse for generating misleading content. To address this barrier, we will establish robust cybersecurity measures to safeguard the LLM from attacks. Moreover, clear usage policies will be implemented and strictly enforced to prevent misuse.
- For-profit, including B-Corp or similar models
We are applying for the Trinity Challenge as it offers an opportunity to secure the essential funding required to rigorously test our proof-of-concept across our four implementation countries. This funding will be instrumental in validating the efficacy of our concept within diverse health programs, particularly in addressing the critical issue of antibiotic regulation and AMR.
By obtaining financial support from this challenge, we will be empowered to undertake crucial documentation processes to uphold data privacy standards and acquire necessary certifications. These steps are essential to ensure the ethical handling of sensitive health data and to comply with regulatory requirements, thereby fostering trust and confidence among stakeholders.
Furthermore, participation in the Trinity Challenge not only provides financial resources but also facilitates invaluable networking opportunities and access to expertise in the global health community. Leveraging these connections will enable us to garner insights, refine our approach, and maximise the impact of our initiative on antibiotic stewardship and broader public health goals.
We are applying because we want to provide community-level data that will be used to measure access, and use of antibiotics in the community by the informal sectors with particular interest on PPMVs.
Our team currently has an existing relationship with academic institutions in Nigeria, and Kenya and we are already collaborating with the Ministries of Health in these countries who are also in charge of the regulatory bodies that we will be working with to validate the conversational AI after training. Our team has existing partnerships with the Nigeria Centre for Disease Control and the Africa CDC; this study builds on these existing relationships, with collaborators drawn from these partners as well.
Our team is exploring additional partnerships with local technology hubs in the implementation countries, who are empowered as local providers of discounted cloud service storage. We envision that partnerships that reduce the total cost of cloud storage services will be key to scaling up our intervention for frontline health workers in other similar low-resource settings.
This solution is also premised on a new relationship with the national bodies coordinating PPMVs in Nigeria, Kenya, the DRC, and Lesotho. The proposed use case here focuses on PPMVs, and the pathway to scale will include an extension of the use case to other frontline health worker cadres, necessitating similar relationships with the associations of those frontline health workers and their communities of practice.